Pearls of Wisdom: Anaphylaxis
Question: Louis is a 37-year-old physician who sustained a large local reaction to wasp envenomation at age 14, followed by an anaphylactic reaction to the next sting at age 25. At age 27, he successfully underwent desensitization to bee venom and achieved complete tolerance to maximum strength venom extract over a 12-month progressive desensitization regimen. His occupation as a physician and outdoor activity profile does not lead to commonplace exposure to bee stings.
An appropriate statement about next steps for him is:
A. Bees? Don’t bother them and they won’t bother you.
B. The risk of bee sting is unpredictable; carry an EpiPen routinely.
C. No further Rx is necessary; immunotherapy is protective.
D. Because he is a physician, no instruction in EpiPen use is necessary.
What is the correct answer?
(Answer and discussion on next page)
Louis Kuritzky, MD, has been involved in medical education since the 1970s. Drawing upon years of clinical experience, he has crafted each year for almost 3 decades a collection of items that are often underappreciated by clinicians, yet important for patients. These “Pearls of Wisdom” often highlight studies that may not have gotten traction within the clinical community and/or may have been overlooked since their time of publishing, but warrant a second look.
Now, for the first time, Dr Kuritzky is sharing with the Consultant360 audience. Sign up today to receive new advice each week.
Answer: The risk of bee sting is unpredictable; carry an EpiPen routinely.
Bee stings cause approximately 40 deaths in the United States each year.1 Species-specific venom immunotherapy is highly effective. I know that because I have suffered both a large local and an anaphylactic reaction to bee stings.
The most recent adverse reaction I experienced occurred while I was a medical student. I was standing outside a local emergency room having a conversation with a friend, having just finished my emergency room shift. As we both leaned up against a fence on the edge of the parking lot, I noticed a flower bush several feet away with a number of happy bees buzzing around them. Unfortunately, “don’t bother the bees and they won’t bother you” didn’t hold true and a bee did sting me.
_______________________________________________________________________________________________________________________________________________________________________
RELATED CONTENT
Bee Sting Relief
Anaphylaxis: 36 Commonsense Ways to Reduce the Risk
_______________________________________________________________________________________________________________________________________________________________________
Within seconds I became short of breath and tachycardic, but being only yards from the entrance to the ER, I walked back in and was promptly and appropriately treated and released.
Several years later, I underwent (successful) desensitization to bee venom. But what does successful mean?
Literature
The literature suggests that venom immunotherapy is very effective.2 That is, the likelihood of a systemic reaction to bee sting is reduced by 90% to 99% after successful immunotherapy. Because near-perfect is not quite the same as perfect, it is still recommended that persons who have sustained a systemic reaction continue to carry an EpiPen. A physician had prescribed an EpiPen for me at the time, but I might characterize the instruction in its use that I received as minimal—after all, I was a physician and should know how to use it, right?
EpiPen Use2

Meet the EpiPen
Over a decade after purchasing my EpiPen, I read an article that reported surprising levels of unfamiliarity of intended users with the EpiPen. A guilty gulp of recognition shamed me into unearthing my own archival EpiPen to make sure I knew how to properly use it.
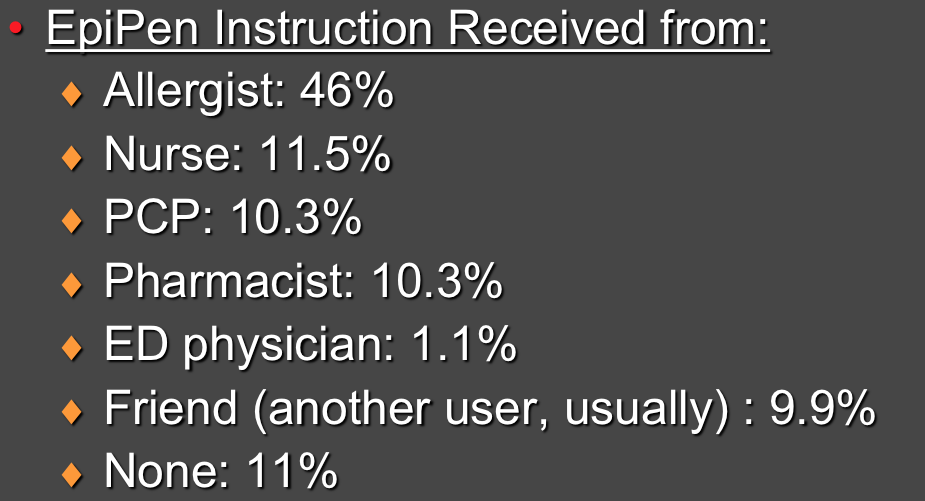
Who Received EpiPen Instructions?2
During the “getting to know you” phase of my first interaction with my EpiPen, I discovered two things:
1. The discolored solution indicated that out-of-date really does mean out-of-date.
2. When one accidentally injects an EpiPen into one’s own thumb, it is not a good thing.
So, after getting over the initial shock of a relatively large-bore needle having just harpooned my thumb, I called the ER for advice. My thumb, by now, was white and cool, as well as sore. Not desirous of displaying the product of my lack of agility to my colleagues, I decided to try and wait out the adrenergic bolus; I soaked my thumb in hot water and restored good circulation and color within an hour or so.
I have told this story at CME meetings before and at this point, I’m surprised when someone doesn’t come up to me afterwards and share a similar story. So what needs to change?
Who Used an EpiPen Correctly?2

One study of venom immunotherapy patients (or their parents) found some room for improvement: 79% had received an EpiPen prescription and 30% said they carried with them every day. When asked to show the interviewer the EpiPen, however, only slightly over half actually had the EpiPen with them and 11% of those had an expired EpiPen on hand.
The persons who had been prescribed an EpiPen had received variable levels of instruction in its use. When asked to demonstrate proper use of the device, less than half properly performed the 3 steps necessary to safely and effectively use the medication.
How to Use an EpiPen3

Similarly, many patients were confused about what to do after a sting: Wait and see? Give the shot immediately? Take an antihistamine?
Strategy After A Re-sting2

What’s the “Take Home”?
Bee stings are serious business for some folks. Many of us, despite having gone through the scare of systemic reactions, are neglectful about keeping our EpiPen around, perhaps lulled into complacency by the very high efficacy of venom immunotherapy. To avoid the Moby Thumb Syndrome (ie, thumb harpooned by needle not intended to go into thumb), make sure to review the step-by-step appropriate use of the EpiPen with every patient (or their parent/caregiver) to ensure safe and effective use—even when the patient is another healthcare provider.
References:
- Asthma and Allergy Foundation of America. What is anaphylaxis? http://www.aafa.org/display.cfm?id=9&sub=21&cont=295. Accessed May 29, 2014.
- Goldberg A, Confino-Cohen R. Insect sting-inflicted systemic reactions: attitudes of patients with insect venom allergy regarding after sting behavior and proper administration of epinephrine. J Allerg
- How to Use Your EpiPen. Mylan Inc. https://www.epipen.com/en/about-epipen/how-to-use-epipen. Accessed May 29, 2014.


