Internal Hernia and Gastric Remnant Perforation After Gastric Bypass
A 30-year-old woman with a distant history of Roux-en-Y gastric bypass (RYGBP) surgery presented to the emergency department with a 2-day history of worsening diffuse abdominal pain radiating to her back. She initially received a diagnosis of pancreatitis based on a lipase level of approximately 9000 U/L.

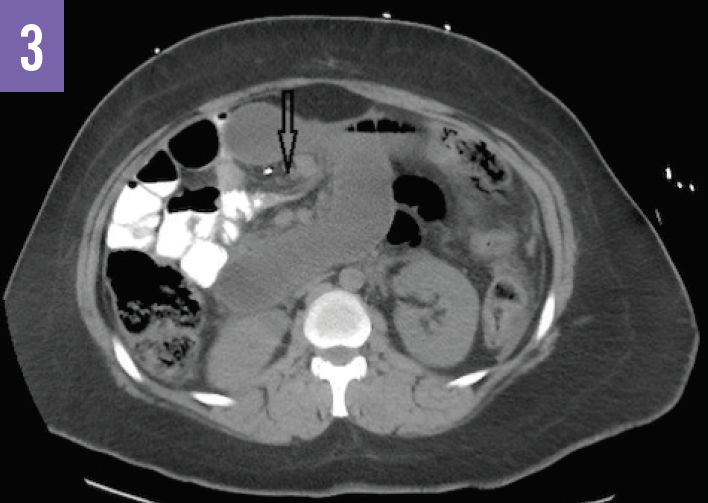
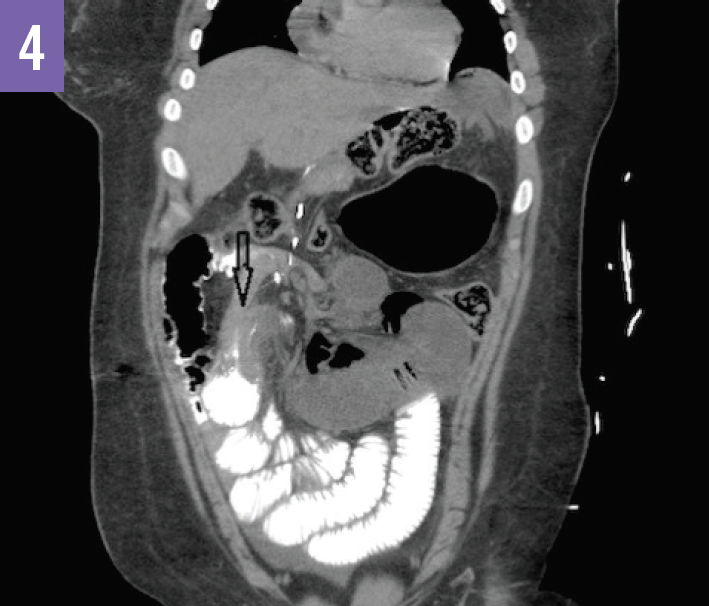
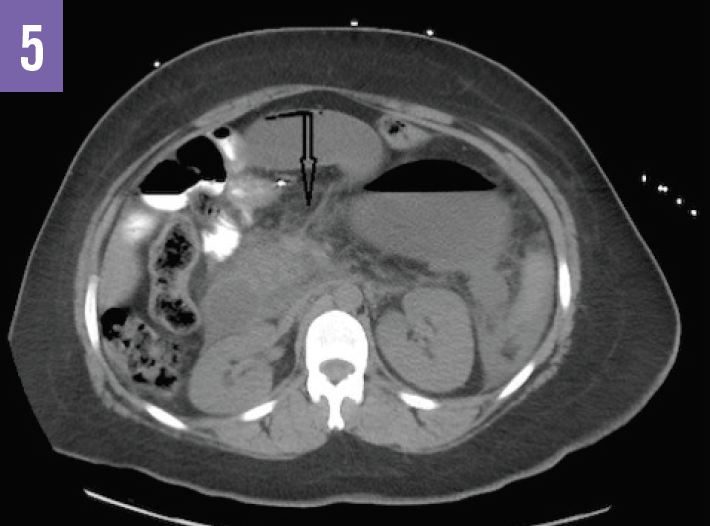
Diagnostic tests. An acute abdominal radiograph series was unremarkable for pneumoperitoneum but demonstrated a gastric air bubble (Figure 1). Computed tomography (CT) of the abdomen and pelvis with oral diatrizoate meglumine and diatrizoate sodium solution contrast medium demonstrated free air under the left hemidiaphragm and gastric pneumatosis (Figure 2), possible obstructions of the bilioenteric limb and within the common channel (Figures 3 and 4), and fat stranding at the pancreatic head (Figure 5).
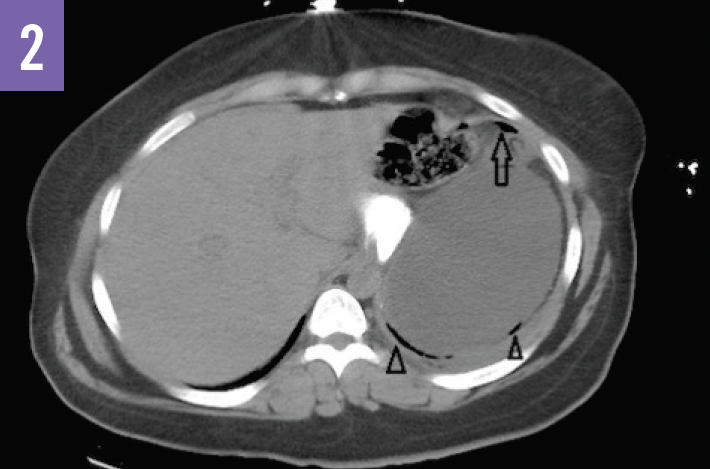
Based on the imaging results, the patient received a diagnosis of internal hernia with perforation of the gastric remnant.
Discussion. Internal hernias occur as a late finding in 3% of RYGBP patients from herniation of small bowel loops through a defect in the transverse mesocolon, small bowel mesentery, or Roux limb.1 Results of initial radiologic studies may be nonspecific, thus necessitating high clinical suspicion to diagnose the condition before bowel ischemia or infarction occurs.2 Abdominal radiographs demonstrating a gastric air bubble are abnormal in bariatric surgery patients and often represent air in the gastric remnant, thus suggesting an internal hernia or distal obstruction.3
The “mesenteric swirl” sign—twisting of the mesenteric vessels or fat at the root of the mesentery—on CT imaging is specific for an internal hernia; however, this finding does not appear in every case and therefore other signs of obstruction, such as segmental dilation and abnormal location of distended bowel, should raise the suspicion for internal hernia.4,5
Treatment for this condition consists of urgent surgical reduction of the strangulated bowel with excision and removal of any necrotic bowel and perforated gastric remnant.
Outcome of the case. The patient was taken to the operating room for emergent reduction of an internal hernia at the jejuno-jejunal anastomosis with a subtotal gastrectomy for a perforated gastric remnant.
References:
- Levine MS, Carucci LR. Imaging of bariatric surgery: normal anatomy and postoperative complications. Radiology. 2014;270(2):327-341.
- Carucci LR, Turner MA, Shaylor SD. Internal hernia following Roux-en-Y gastric bypass surgery for morbid obesity: evaluation of radiographic findings at small-bowel examination. Radiology. 2009;251(3):762-770.
- Luber SD, Fischer DR, Venkat A. Care of the bariatric surgery patient in the emergency department. J Emerg Med. 2008;34(1):13-20.
- Iannuccilli JD, Grand D, Murphy BL, Evangelista P, Roye GD, Mayo-Smith W. Sensitivity and specificity of eight CT signs in the preoperative diagnosis of internal mesenteric hernia following Roux-en-Y gastric bypass surgery. Clin Radiol. 2009;64(4):373-380.
- Martin LC, Merkle EM, Thompson WM. Review of internal hernia: radiographic and clinical findings. AJR Am J Roentgenol. 2006;186(3):703-717.


