Sagittal Craniosynostosis With Scaphocephaly
AUTHORS:
Syed A. A. Rizvi, PhD, MS, MBA
Hampton University School of Pharmacy, Hampton, Virginia
Zafar Qureshi, MD
UHI CommunityCare Clinic, Miami, Florida
Elizabeth Mancuso, PA-S
Keiser University, Fort Lauderdale, Florida
Alexis Kinloch, PA-S
Keiser University, Fort Lauderdale, Florida
CITATION:
Rizvi SAA, Qureshi Z, Mancuso E, Kinloch A. Sagittal craniosynostosis with scaphocephaly. Consultant. 2019;59(11):339-340.
A 3-month-old boy was brought to the clinic by his mother with concern for abnormal head shape. He had been born at term via spontaneous vaginal delivery, without any complications.
Physical examination. The patient was awake, alert, on room air, and did not appear distressed. He was able to move all 4 extremities evenly with good strength. His axillary temperature was 36.3°C, blood pressure was 89/55 mm Hg, pulse was 121 beats/min, and respiratory rate was 24 breaths/min. The patient’s height was 610 cm, and he weighed 6 kg.
Diagnostic tests. Axial thin-section computed tomography (CT) images of the brain were obtained from the base of the skull to the vertex without intravenous contrast (Figure 1). Coronal reconstructed images were also obtained (Figure 2). Sagittal craniosynostosis with scaphocephaly was noted. The lambdoid and sutures were patent.
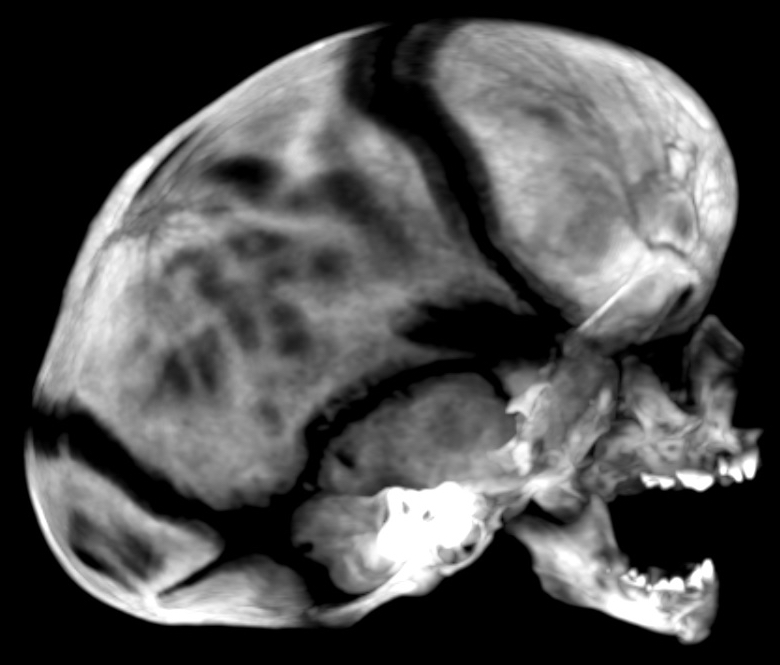
Figure 1. CT scan of the skull.

Figure 2. Preoperative 3-dimensional CT reconstruction of the head showing scaphocephaly (A) and sagittal craniosynostosis (B and C).
The patient was admitted for endoscopic cranial vault surgery to be performed in conjunction with plastic surgery. Postoperatively, the child was monitored in the pediatric intensive care unit for 24 hours. The Jackson-Pratt drain was removed on postsurgical day 2 without incidence (Figure 3).

Figure 3. Postoperative image of the patient’s head with digital surface imaging, left lateral view (left) and right lateral view (right).
The diet was easily advanced, and the pain was well controlled. The patient was eating and sleeping well and was discharged from the hospital on day 4.
Discussion. Craniosynostosis (the most common nonsyndromic monosynostosis) is the premature fusion of cranial sutures before brain growth is complete, and it can lead to skull deformities and neurological abnormalities. Craniosynostosis can develop in utero and present in infancy or after birth due to mechanical or metabolic causes and commonly presents at approximately 2 years of age.1,2 Its prevalence is 3.1 to 6.4 per 10,000 live births, and predominantly affects boys (70% to 90% of cases).3,4 It has been reported that approximately 21% of cases are a result of single gene mutations or chromosomal abnormalities, and very rarely both.5,6
Primary craniosynostosis results from genetic mutations in the fibroblast growth-factor receptors and is associated with Apert, Crouzon, Pfeiffer, Jackson-Weiss, Beare-Stevenson cutis gyrate, and Muenke syndromes.5,7 Secondary craniosynostosis can result from several disorders such as hypercalcemia, hypophosphatasia, hyperthyroidism, vitamin D deficiency, renal osteodystrophy, sickle cell disease, thalassemia, and Hurler syndrome.7,8
Treatment involves surgical intervention and should start early. For our patient, an endoscopic method was employed, along with postoperative orthosis to ensure proper skull growth, since it is a less-invasive technique that is commonly used for surgical correction of craniosynostosis among children.9,10
References:
- Vega RA, Opalak C, Harshbarger RJ, et al. Hypophosphatemic rickets and craniosynostosis: a multicenter case series. J Neurosurg Pediatr. 2016;17(6):694-700.
- Kabbani H, Raghuveer TS. Craniosynostosis. Am Fam Physician. 2004;69(12):2863-2870.
- Cornelissen M, den Ottelander B, Rizopoulos D, et al. Increase of prevalence of craniosynostosis. J Craniomaxillofac Surg. 2016;44(9):1273-1279.
- Komotar RJ, Zacharia BE, Ellis JA, Feldstein NA, Anderson RCE. Pitfalls for the pediatrician: positional molding or craniosynostosis? Pediatr Ann. 2006;35(5):365-375.
- Johnson D, Wilkie AOM. Craniosynostosis. Eur J Hum Genet. 2011;19(4):369-376.
- Wilkie AOM, Byren JC, Hurst JA, et al. Prevalence and complications of single gene and chromosomal disorders in craniosynostosis. Pediatrics. 2010;126(2):e391-e400.
- Khanna PC, Thapa MM, Iyer RS, Prasad SS. Pictorial essay: the many faces of craniosynostosis. Indian J Radiol Imaging. 2011;21(1):49-56.
- Hwang S-K, Park K-S, Park S-H, Hwang SK. Update of diagnostic evaluation of craniosynostosis with a focus on pediatric systematic evaluation and genetic studies. J Korean Neurosurg Soc. 2016;59(3):214-21
- Murad GJA. Clayman M, Seagle MB, White S, Perkins LA, Pincus DW. Endoscopic-assisted repair of craniosynostosis. Neurosurg Focus. 2005;19(6):E6.
- Proctor MR. Endoscopic craniosynostosis repair. Transl Pediatr. 2014;3(3):247-258.


