Peer Reviewed
Isolated Unilateral Oculomotor Nerve Paresis: An Uncommon Presentation of Midbrain Stroke
AUTHORS:
Zekarias Asnake, MD1,2 • Jawad Noor, MD1,2 • Manjot Malhi, MD1,2 • George Cockey, MD, PhD1,2
AFFILIATIONS:
1University of Central Florida College of Medicine, Orlando, Florida
2North Florida Regional Medical Center, Gainesville, Florida
CITATION:
Asnake Z, Noor J, Malhi M, Cockey G. Isolated unilateral oculomotor nerve paresis: an uncommon presentation of midbrain stroke. Consultant. 2021;61(3):e20-e21. doi:10.25270/con.2020.07.00013
Received May 8, 2020. Accepted July 10, 2020. Published online July 30, 2020.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
George Cockey, MD, PhD, Assistant Professor, University of Central Florida College of Medicine, 6850 Lake Nona Blvd, Orlando, FL 32827 (ghcgolfer@msn.com)
Isolated unilateral oculomotor nerve paresis is a rare presentation of midbrain cerebrovascular accident. This report describes a case of isolated unilateral oculomotor nerve paresis resulting from a tiny lacunar infarct in the midbrain. Given the patient’s poorly controlled type 2 diabetes, ischemic oculomotor nerve palsy was most likely etiology. However, diffusion-weighted magnetic resonance imaging (MRI) of the brain revealed a subacute lacunar infarction in left midbrain.
Case report. A 68-year-old woman with a history of poorly controlled type 2 diabetes, hypertension, coronary artery disease, and kidney failure on hemodialysis presented to the hospital with sudden-onset dizziness and unilateral diplopia of one day’s duration. She reported that the dizziness was aggravated by standing and resolved with closing her left eye. She denied having any paresthesia or weakness.
Physical examination. At presentation, she was afebrile and had a blood pressure of 137/88 mm Hg and a pulse rate of 84 beats/min. Physical examination demonstrated an adult woman of average build and size lying comfortably in bed with no signs of ocular swelling or injury. Cranial nerve examination revealed ptosis of the left eye, loss of left eye adduction, and bilateral reactive pupils. Otherwise, her neurologic examination findings (including cranial nerve function, sensory function, motor function, and cerebellar examination findings) were all normal.
Diagnostic tests. Results of laboratory tests were largely unremarkable except for mild anemia (hemoglobin level, 9.8 mg/dL), thrombocytopenia (platelet count, 115 × 103/µL), and an elevated creatinine level (6.87 mg/dL) consistent with kidney failure. Results of transthoracic echocardiography showed an ejection fraction of 25% to 30% with no wall motion abnormalities or atrial septal defect. Findings of computed tomography (CT) of the brain and CT angiography of the head and neck were unremarkable. Diffusion-weighted and T2-weighted MRI scans of the brain revealed a tiny subacute lacunar infarction in the left midbrain (Figures 1 and 2).

Figure 1. Diffusion-weighted MRI of the brain showing a punctate focus of restricted diffusion (arrow) in the left midline area of the midbrain consistent with a small subacute lacunar infarction.
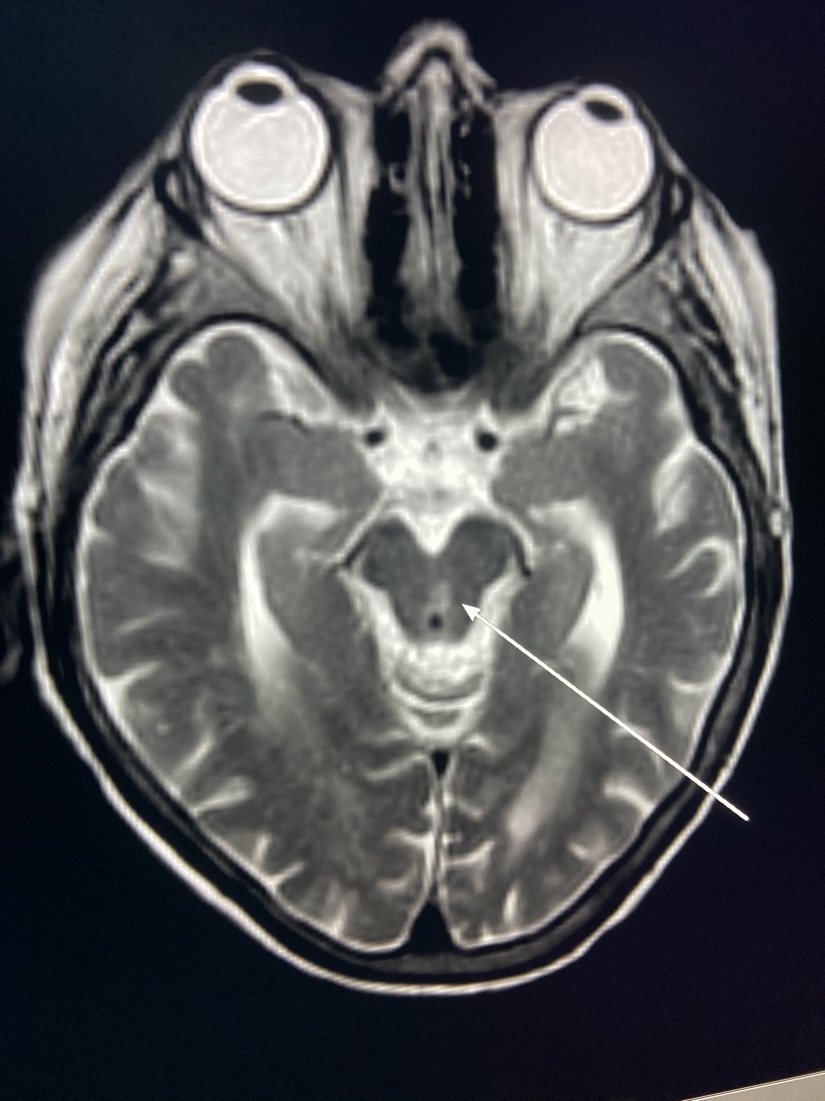
Figure 2. T2-weighted MRI of the brain showing a punctate hyperintensity (arrow) in the left midline area of the midbrain consistent with a small subacute lacunar infarction.
Discussion. The oculomotor nerve arises from two nuclei, the Edinger-Westphal nucleus and the oculomotor nucleus, in the midbrain just inferior to the mammillary bodies.1 The nerve goes through the lateral wall of the cavernous sinus into the orbit through the superior orbital fissure and divides into superior and inferior branches.1,2 The superior branch innervates the levator palpebrae and superior rectus muscles, while the inferior branch supplies the following intrinsic eye muscles: the medial and inferior rectus muscles, the inferior oblique, and the pupillary sphincter.2
The oculomotor nerve has both somatic and autonomic functions. Its somatic functions involve elevation, adduction, and depression of eye by extraocular muscles, while the levator palpebrae superioris is involved in upper eyelid elevation. Its autonomic function involves accommodation by the ciliary muscle and miosis by the sphincter pupillae.1
The fibers within the oculomotor nerve are organized in a specific pattern. In the ventral midbrain, fibers supplying the sphincter pupillae and the inferior rectus are on the medial aspect of the oculomotor nerve, while those supplying the medial rectus, levator palpebrae superioris, superior rectus, and inferior oblique muscles are on lateral side of oculomotor nerve.3 At the level of the interpeduncular fossa, where the ventral midbrain divides, the medial part of the oculomotor nerve lies on the anterior surface, while the lateral part runs more deeply. The deeper side of the oculomotor nerve is supplied by vasa vasorum and is more susceptible to ischemia.1
The oculomotor nerve can be damaged anywhere along its course from the midbrain to the orbit. The most common cause of oculomotor nerve paresis is microvascular ischemia, followed by inflammatory diseases, aneurysm, cerebrovascular accident, trauma, and neoplasm.4 Oculomotor nerve paresis can be divided into isolated oculomotor nerve paresis and nonisolated oculomotor nerve paresis. Nonisolated oculomotor paresis presents with additional neurological deficit. Midbrain strokes involving the levator palpebrae, superior rectus, and inferior oblique muscles are relatively common but typically present with other neurological symptoms (eg, focal motor weakness, dysarthria).
One group of authors studied 5 cases of isolated oculomotor nerve paresis resulting from pure midbrain stroke.3 The pupillary sphincter and inferior rectus muscles were selectively spared in those cases.3 The oculomotor fibers that supply the levator palpebrae, superior rectus, and inferior oblique muscles are more prone to ischemia compared with those that supply the pupillary sphincter and inferior rectus muscles, and this explains the common pattern associated with midbrain ischemia.
In our patient, who presented with a sudden onset of symptoms, microvascular insult topped the differential diagnosis list. After a thorough history, physical examination, and neuroimaging studies, our patient was found to have sustained a small midbrain stroke mimicking oculomotor nerve mononeuropathy. Isolated ipsilateral oculomotor palsy with sparing of the pupillary sphincter was consistent with the findings of a previously reported case.4
Our review of the literature revealed that ischemia preferentially involves the oculomotor fibers innervating the levator palpebrae, superior rectus, and inferior oblique muscles. Although midbrain ischemia commonly presents with focal motor weakness and diplopia, unilateral oculomotor paresis sometimes can be the only manifestation of midbrain ischemia and should be considered in patients presenting with oculomotor nerve mononeuropathy.
Our patient was managed conservatively with aspirin and a statin and an alternating eye patch to treat her diplopia.
REFERENCES:
- Joyce C, Le PH, Peterson DC. Neuroanatomy, cranial nerve 3 (oculomotor). StatPearls. Updated May 24, 2020. Accessed July 14, 2020. https://www.ncbi.nlm.nih.gov/books/NBK537126/
- Bhatti MT, Eisenschenk S, Roper SN, Guy JR. Superior divisional third cranial nerve paresis: clinical and anatomical observations of 2 unique cases. Arch Neurol. 2006;63(5):771-776. doi:10.1001/archneur.63.5.771
- Amano Y, Kudo Y, Kikyo H, et al. Isolated unilateral oculomotor paresis in pure midbrain stroke. J Neurol Sci. 2015;351(1-2):191-195. doi:10.1016/j.jns.2015.03.012
- Choi K-D, Choi SY, Kim J-S, et al. Acquired ocular motor nerve palsy in neurology clinics: a prospective multicenter study. J Clin Neurol. 2019;15(2):221-227. doi:10.3988/jcn.2019.15.2.221


