Peer Reviewed
Getting a Grip on Hand Knob Stroke
AUTHORS:
Analiese Wagner, DO
Department of Emergency Medicine, Rowan University School of Osteopathic Medicine/Jefferson Health, Stratford, New Jersey
Kevin Dwyer, DO
Department of Emergency Medicine, Virtua Healthcare System, Voorhees, New Jersey
James Espinosa, MD
Department of Emergency Medicine, Rowan University School of Osteopathic Medicine/Jefferson Health, Stratford, New Jersey
Alan Lucerna, DO
Department of Emergency Medicine, Rowan University School of Osteopathic Medicine/Jefferson Health, Stratford, New Jersey
CITATION:
Wagner A, Dwyer K, Espinosa J, Lucerna A. Getting a grip on hand knob stroke [published online February 5, 2020]. Consultant360.
A 65-year-old man presented to the emergency department (ED) for the evaluation of right upper-extremity paresthesias of 1 week’s duration. He also reported clumsiness of the right hand that had worsened over the preceding 48 hours. In addition, he reported a nondescript, generalized headache with no associated vision changes, fevers, or neck pain. He denied arm pain and had otherwise been in his usual state of health. He had seen his primary care physician 2 days prior, had received a diagnosis of peripheral neuropathy, and had been started on gabapentin.
The patient’s history was significant for seizures, anxiety, and chronic obstructive pulmonary disease. He had a 30 pack-year smoking history and drank alcohol socially. His family history was significant for coronary artery disease in both parents and cerebrovascular accident (CVA) in his father.
On arrival to the ED, his vital signs were as follows: blood pressure, 143/98 mm Hg; heart rate, 84 beats/min; respiratory rate, 16 breaths/min; oral temperature 36.7°C; and oxygen saturation, 100% on room air. While he did not have a prior primary diagnosis of hypertension, he was noted to be hypertensive during his ED course.
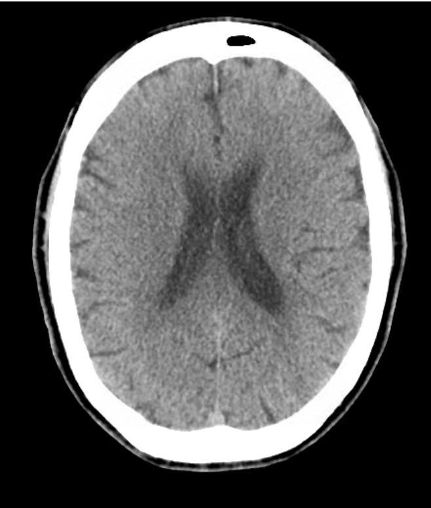
On examination, he was noted to have dysmetria of the right hand, as well as difficulty with fine motor movement and with pincer grasp. The remainder of his neurological examination and physical examination findings were within normal limits. Computed tomography (CT) imaging of the brain findings were unremarkable (Figure 1).
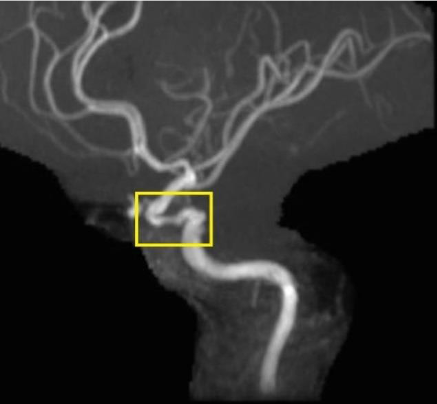
Basic laboratory test results were also normal. Aspirin was administered, and the patient was admitted for additional workup to differentiate a central process vs a peripheral process as the cause of the symptoms. At admission, the patient underwent magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA) of the brain and neck and was found to have stenosis of his left internal carotid artery within the cavernous sinus portion, as well as an acute infarction involving the left posterior middle cerebral artery territory (Figures 2 and 3).

He was evaluated by a neurologist, whose diagnosis was hand-knob stroke. The patient did well during his stay and was discharged on aspirin and statin therapy. The patient was referred for continued neurologist follow-up.
DISCUSSION
This patient presented with 1 week of symptoms that were isolated to his distal right upper extremity. His symptoms seemed to be peripheral in nature, and the associated neurologic deficits appeared to be very subtle. His presentation was typical of a stroke in the hand knob region.
Using functional MRI, Yousry and colleagues1 were able to localize motor function of the hand to a knob-shaped area in the precentral gyrus. This area proved to be a reliable landmark for identifying the precentral gyrus.1 Takahashi and colleagues2 observed similar findings in their 2002 study of 5 patients with upper extremity neurologic deficits; their patients had MRI evidence of lesions in the knob area.
Imaging studies performed on our patient showed hemodynamically significant narrowing of the left internal carotid artery and an infarct in the left middle cerebral artery territory; this too is consistent with a hand knob stroke. Gass and colleagues3 studied 14 patients with distal upper extremity paresis, all with lesions located in the hand knob area. In this study, diffusion-weighted images were compared with perfusion-weighted images, and the authors determined that obstruction of the middle cerebral artery was a common source of the infarct.3 Similar to the findings in our patient’s case, another study by Peters and colleagues4 showed that stenosis and atherosclerosis of the internal carotid artery were common. Hypertension was also a common risk factor in that study.4 In both of these studies, patients had good functional outcomes. Both studies also suggest that embolic sources for occlusion are more common.
Several case reports have been published regarding the similarities of a hand knob stroke with a peripheral lesion. Presentations consistent with ulnar nerve and median nerve palsies as well as anterior interosseous syndrome (AINS) have been described. One case study described a patient with difficulty with thumb-index finger pinching, typical of AINS, who was found to have a point lesion in the hand knob area on MRI after initial workup did not identify a peripheral source.5 In a similar case study, on close examination the patient had very subtle deficits of surrounding muscle groups that was inconsistent with AINS or an isolated median nerve palsy, and further studies identified a CVA.6 Both sensory and motor deficits in an ulnar nerve distribution have also been reported.7 In most cases, acute onset of symptoms occurs. Careful attention to the mechanism can also help distinguish the 2 entities—ie, trauma in the case of AINS or painful nocturnal symptoms in carpal tunnel syndrome.6 Detailed physical examination is important, as well, and any inconsistency that does not match a suspected peripheral pattern should prompt a search for a central cause.
Cortical strokes involving the hand knob area are well described; however, the true incidence is unknown. Current available case studies have small population sizes, making generalization about this type of stroke difficult. Peters and colleagues4 reviewed 29 cases representing less than 1% of patients in their stroke unit. Likewise, Alstadhaug and Sjulstad8 studied 17 patients comprising approximately 1.5% of their patients with stroke.
CONCLUSION
Infarcts involving the hand knob area are uncommon and have more subtle findings than typical CVAs. Although clinical outcomes appear to be good based on current case studies, treatment of hand knob stroke and a peripheral neuropathy are different. The timing of onset, a detailed history and physical examination, and assessment of a patient’s risk factors for CVA are important considerations in order to make that distinction. Most importantly, simply having the knowledge that this entity exists can help prevent misdiagnosis as a peripheral lesion and guide the patient toward appropriate care.
REFERENCES:
- Yousry TA, Schmid UD, Alkadhi H, et al. Localization of the motor hand area to a knob on the precentral gyrus. A new landmark. Brain. 1997;120(pt 1):141-157. doi:10.1093/brain/120.141
- Takahashi N, Kawamura M, Araki S. Isolated hand palsy due to cortical infarction: localization of the motor hand area. Neurology. 2002;58(9):1412-1414. doi:10.1212/wnl.58.9.1412
- Gass A, Szabo K, Behrens S, Rossmanith C, Hennerici M. A diffusion-weighted MRI study of acute ischemic distal arm paresis. Neurology. 2001;57(9):1589-1594. doi:10.1212/wnl.57.9.1589
- Peters N, Müller-Schunk S, Freilinger T, Düring M, Pfefferkorn T, Dichgans M. Ischemic stroke of the cortical “hand knob” area: stroke mechanisms and prognosis. J Neurol. 2009;256(7):1146-1151. doi:10.1007/s00415-009-5104-8
- Granziera C, Kuntzer T, Vingerhoets F, Cereda C. Small cortical stroke in the “hand knob” mimics anterior interosseous syndrome. J Neurol. 2008;255(9):1423-1424. doi:10.1007/s00415-008-0930-7
- Manjaly Z-M, Luft AR, Sarikaya H. An unusual cause of pseudomedian nerve palsy. Case Rep Neurol Med. 2011;2011:474271. doi:10.1155/2011/474271
- Ueno T, Tomiyama M, Haga R, et al. Ulnar nerve palsy-like motor and sensory loss caused by a small cortical infarct. J Stroke Cerebrovasc Dis. 2012;21(8):903.e3–903.e903004. doi:10.1016/j.jstrokecerebrovasdis.2011.02.008
- Alstadhaug KB, Sjulstad A. Isolated hand paresis: a case series. Cerebrovasc Dis Extra. 2013;3(1):65-73. doi:10.1159/000350708


