Coronary Artery Stents: From the Beginning to the Present
AUTHORS:
Suvash Shrestha, MBBS1 • Jignesh Patel, MD2 • Gerald Hollander, MD2 • Jacob Shani, MD2
AFFILIATIONS:
1Department of Cardiology, James J. Peters VA Medical Center, Bronx, New York
2Department of Cardiology, Maimonides Medical Center, Brooklyn, New York
CITATION: Shrestha S, Patel J, Hollander G, Shani J. Coronary artery stents: from the beginning to the present. Consultant. 2020;59(6):e1. doi:10.25270/con.2020.03.00024
Received September 17, 2019. Accepted October 9, 2019.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE: Suvash Shrestha, MBBS, James J. Peters VA Medical Center, 130 W Kingsbridge Rd, Bronx, NY 10468 (suvashsht@gmail.com)
ABSTRACT: Coronary angioplasty is now one of the most widely performed cardiac procedures in the world. It has become routine to open an occluded artery, but this was not the case just a few decades ago. Cardiac events were considered bolts of thunder, not knowing who and when they will strike. There was neither an understanding of the cardiac pathophysiology nor any treatment options. There was almost nothing physicians could do except to have the patient rest and observe, hoping for the best. Led by some brilliant minds of the 20th century, we have come a long way in the journey into the heart. In 1929, Werner Forssmann threaded a catheter into his own heart. F. Mason Sones pioneered coronary imaging. Charles T. Dotter used catheters to open occluded peripheral vessels, and Andreas Gruentzig took it further and initiated balloon angioplasty in the coronary arteries. We will always remain indebted to these people and many other whose relentless work and ingenuity have advanced the field of interventional cardiology to the current state. Here we provide a brief overview of the lives of the pioneers of interventional cardiology and the evolution of coronary artery stents.
KEYWORDS: Coronary angiography, coronary artery stent, myocardial infarction
In 1955, during a round of golf, President Dwight D. Eisenhower experienced a myocardial infarction (MI). However, it would not be diagnosed until many hours later, when his chest pain became more intense and excruciating. He would be treated with oxygen, amyl nitrate, papaverine, morphine, and heparin and for several weeks be confined to in-hospital bed rest hoping for the best.1,2 Such was the predicament of patients with coronary artery disease (CAD) not long ago. The hours and days after the coronary event were treacherous and the outcome often grim. Such an event neither was understood nor was any effective treatment available for it. But things have changed; it has become routine to open occluded arteries in minutes. Indeed, we have come a long way in the journey into the heart, led by some brilliant minds who we will always remain indebted to.
A LOOK INTO THE HISTORY
Werner Forssmann (1904–1979)3-6
The journey into the coronary arteries started with Werner Forssmann. He went to Berlin’s prestigious Friedrich Wilhelm University and was always fascinated by the human heart. In 1929, he came up with the wild idea of inserting a catheter into the heart to inject medications. It was a radical idea, and no institution would give him permission to try anything of that sort. Undeterred, he decided to proceed anyway, least worried about the consequences. He enlisted a nurse, Gerda Ditzen, to assist him. He anesthetized his own left elbow, made a quick incision, opened a vein, and pushed a urethral catheter into his own arm. He twisted it deeper, and he had Ditzen help him to the basement radiology department, where he took images with the catheter inside his heart.3-5
Forssmann himself could not pursue cardiac catheterization any further, but years later, in the late 1930s, his idea was picked up by André F. Cournand and Dickinson W. Richards at Columbia University in New York. They refined the technique and used it to make crucial measurements in the heart. In 1956, they along with Forssmann were jointly awarded the Nobel Prize in Physiology or Medicine.6 The catheter technique soon became the standard method to measure intracardiac pressures. But the coronary tree and its intricate branches would continue to remain elusive for some time.
F. Mason Sones (1919–1985)3
Cardiac catheterization eventually paved the path for coronary angiography. F. Mason Sones completed his residency at Henry Ford Hospital in Detroit and joined the Cleveland Clinic in 1950. He was brilliant and relentless and spent most of his time in the hospital. He could skillfully maneuver diagnostic catheters into the aortic trunk arteries and was able to produce very intricate images.3
In his laboratory on October 30, 1958, Sones inserted a diagnostic catheter into the ascending aorta of a young patient. Upon Sones’ instruction, his fellow injected a shot of dye to illuminate the aorta. Unexpectedly, the small catheter whipped like an uncontrolled garden hose and flipped into the patient’s right coronary artery, injecting all of the dye deep in the artery. This had never been attempted before—the prevailing fear was that the nonoxygenated angiographic dye would cut off oxygen delivery, resulting in ventricular fibrillation. For few seconds, Sones felt that he was going to lose his patient. Instead, to his pleasant surprise, the patient remained fine throughout, and in addition, a nice picture of the coronary arteries resulted. Sones triumphantly declared, “We just revolutionized cardiology!”3 And, indeed he did.
Emboldened by the unexpected incident and outcome, Sones began designing special catheters with an open tapered tip and sieve-like opening on the shaft so that the catheter would not obstruct the vessel. Coronary angiography soon became a safe and routine procedure to evaluate CAD.3 However, manipulating a catheter into tiny openings of the coronary arteries required a lot of practice. Melvin P. Judkins, who had studied with Sones, modified the technique and developed special J-shaped catheters that made catheterization of the coronary arteries easier, with minimal manipulation.7 Coronary angiography revolutionized the understanding of CAD and ushered in a new era of coronary intervention.
Charles T. Dotter (1920–1985)8-10
Charles T. Dotter was an eccentric, a free-thinker, a genius who developed numerous ways to diagnose and treat vascular disease.8 He was chairman of the radiology department at the University of Oregon in Portland. He had spent some time at Karolinska Institute in Sweden with Sven-Ivar Seldinger, who is famous for his technique of threading the catheter into the blood vessels—“needle in, wire in, needle out, catheter over the wire.”9 An avid and fearless mountain climber, Dotter thrived on challenges and adventure. He felt that, in addition to the diagnostic purpose, the catheter technique could have further implications, including opening occluded vessels. He experimented with different materials—guitar strings, piano wires, and other cables—and developed his own catheters, as well.
On January 16, 1964, Dotter had performed an arteriogram on the left leg of an 83-year-old woman with diabetes who had a nonhealing foot ulcer and gangrenous toes. Her surgeons had insisted upon amputation of the foot, as they thought her poor circulation was beyond repair. But the woman adamantly refused. So, Dotter saw an opportunity and offered her a procedure that had never before been done. She had short segmental occlusion of the superficial femoral artery, which he felt would be ideal for his dilating catheters. He threaded a guide wire into the plaque blockage and followed it with a small-bore catheter, and then channeled larger and larger catheters through the plaque, just like wedging. Almost miraculously, the woman’s cold leg turned warm and hyperemic. Radiographs showed improved blood flow, and within weeks, the woman’s ulcer had healed, and the pain had resolved.10
Encouraged, Dotter began performing the transluminal dilatation more frequently—which was called “Dottering.” This laid the foundation for another free thinking, innovative genius who saw new possibilities for Dotter’s catheters and, with improvisation of his own, revolutionized the treatment of CAD.
Andreas Gruentzig (1939–1985)3,11,12
Andreas Gruentzig was born during World War II and grew up in East Germany before escaping to West Germany at age 18. He completed his medical undergraduate program in Heidelberg and joined University Hospital of Zurich in 1969. Just before moving to Zurich, Gruentzig had attended a lecture on “Dottering” and was immediately fascinated with the technique, but he also felt it was crude and needed refinements, since it carried a high risk of vascular injuries, dislodging, and embolization of the plaque leading to acute distal occlusion. In his wild and revolutionary imagination, Gruentzig came up with the idea of mounting a balloon at the tip of the catheter to open an occluded blood vessel.
It was 1972, and his idea was totally eccentric at the time, and no one showed much interest and support except his wife, Michaela, and his secretary, Maria Schlumpf. He had no laboratory space and no funding for his research, so he used his kitchen as the work area. For the next 2 years, almost every evening, he and his wife and Schlumpf worked on his catheters at his kitchen table. His idea was to mount a balloon on the tip of the catheter, which he could inflate to force open a closed vessel. It was not an easy task, and they faced numerous technical problems—the leaking of air, balloons losing physical integrity, asymmetrically expanding balloons, and many others. But he persevered and improvised. Night after night, he tried different materials, different shapes, and different designs. After hundreds of trials and errors, he saw some hopeful results. His techniques for fabricating balloons steadily improved, and he tried his design in animal models and diseased arteries from cadavers; eventually, he felt ready to try it on a human patient.
In February 1974, his moment of truth arrived: A 67-year-old man who was incapacitated by lower extremity pain upon walking came to his clinic. The man had stenosis in his major iliac vessel. With meticulous preparation, under x-ray guidance, Gruentzig pushed his catheter and inflated the balloon, the diseased vessel widened splendidly, and the patient’s pain resolved immediately.
Encouraged by this success, he eyed coronary obstruction as his next challenge. Coronary arteries, however, were a different territory. Nobody knew what would happen when a balloon was inflated in a coronary artery, such as possible sudden fibrillation or spasm and closure of the blood vessel. Furthermore, Gruentzig’s catheters were relatively crude. He met with a number of manufacturers and engineers and kept refining the design of his catheters while waiting for an opportunity to use them in the human body.
Then, in 1977, Dolf Bachmann, a 38-year-old insurance salesman, sought medical help for chest pain. Angiography showed a localized narrowing of his left anterior descending artery. But Bachmann refused to undergo then-standard coronary artery bypass grafting (CABG). This provided Gruentzig with a chance to make his move. On September 16, 1977, Bachmann was wheeled into the catheterization laboratory; surgeons were on standby, ready to open his chest should a disaster unfold. Gruentzig went in through the groin and slowly advanced his catheter over a guide wire into the heart and on to the diseased artery. What takes less than a minute now took 45 long minutes. He finally managed to push the catheter forward through the middle of the plaque. He inflated the balloon and held the pressure for 15 long, nervous seconds. To everyone’s relief, electrocardiography recordings remained stable and steady. Bachmann showed no signs of pain. Radiographic images showed that the artery was open. It was a big success, a historic achievement in medicine. Soon, Gruentzig was able to reproduce the results among other cases, and he made headlines. “Medical Sensation: Balloon Treatment Against Heart Attacks,” a Swiss newspaper reported on its front page on February 7, 1978.3
THE RISE OF CORONARY ANGIOPLASTY
Soon, cardiologists from all over the world flocked to Zurich to witness and learn this new technique. In the beginning, Gruentzig was very careful in selecting his patients and promoted balloon angioplasty only to control crippling chronic chest pain rather than to control evolving MIs. In 1979, Gruentzig left Zurich for Emory University in Atlanta, where he felt he could better nurture his invention. He continued to teach more physicians, leading to a new generation of specialists who called themselves interventional cardiologists. On October 27, 1985, Gruentzig died when the twin-engine plane he was piloting crashed in Georgia. Gruentzig was only 46 at his death, but his legacy continues, and his procedure continues to save millions of lives every year.
Over the years, Gruentzig had trained many followers, including Geoffrey O. Hartzler.13 Hartzler was similar to Gruentzig in that he was also fearless, ambitious, and eccentric. In 1980, he shocked the medical world by employing angioplasty in an attempt to demolish an MI as it emerged, and in a way ushered in a new direction in angioplasty. Also, impatient with the shortcomings of Gruentzig’s device, Hartzler began molding better curves into the stiff end of the catheter so that it would slide more easily into place. He also defied the notion that multivessel disease should only be treated with CABG. If the new balloon procedure worked in one vessel, he reasoned, why shouldn’t it succeed in two or three in sequence?
Hartzler kept pushing the boundaries and claimed that the only indication for bypass surgery is failed angioplasty, which was a very brave and bold statement in that era. Although this statement was not entirely correct, early trials comparing angioplasty with surgical procedures, such as the Bypass Angioplasty Revascularization Investigation (BARI),14 the Randomized intervention Treatment of Angina (RITA),15 the Coronary Angioplasty vs Bypass Revascularization Investigation (CABRI),16 the German Angioplasty Bypass Surgery Investigation (GABI),17 and Emory Angioplasty vs Surgery Trial (EAST)18 did show that in selected patients, coronary angioplasty would result in survival comparable with CABG.
Over time, what started in Gruentzig’s kitchen became one of the most clinically significant and frequently performed procedures in medical history. With time, it has gone through several modifications and improvements. Balloon technology has advanced, resulting in better interaction between the balloon surface and the plaque. Cutting balloons with microblades running parallel to the longitudinal axis and scoring balloons with blade running either helically or longitudinally were devised in a quest for more-controlled plaque dissection. While the cutting balloon itself did not reduce the rate of restenosis, it was associated with procedural advantages such as the use of fewer balloons, a low incidence of balloon slippage, and less requirement for additional stenting.19,20
THE INTRODUCTION OF STENTS
As the number of angioplasty procedures increased around the world, it came to attention that many patients’ arteries gradually constricted weeks or months after the procedure. Some even had abrupt vessel closure hours to days after angioplasty. Early studies reported restenosis rates varying from 12% to 48%.21 To address these issues, stents were developed that would maintain vessel patency following angioplasty.
The first stents were implanted in 1986 in Switzerland by Ulrich Sigwart and in France by Jacques Puel.22 These self-expanding mesh designs were followed by coil stents, first implanted at Emory University Hospital in 1987, and slotted tube designs, first implanted in São Paulo, Brazil, the same year.5 Studies showed superior immediate results and greater event-free survival with stents compared with conventional balloon angioplasty. The overall restenosis rates were reduced by approximately 10%.23,24 Stenting soon became the standard of care.
STENT STRUCTURE AND COMPOSITION
All stents consist of an underlying scaffold, and most of them are balloon-expandable. Early stents primarily used stainless steel. Newer stents use cobalt-chromium and platinum-chromium alloys, which have greater radial strength. This allowed the stent struts to become thinner (approximately 75 µm, compared with 100-150 µm for most stainless steel–based designs). This was a significant improvement, and trials confirmed that stents with thin struts have lower rates of restenosis than those with thick struts.25
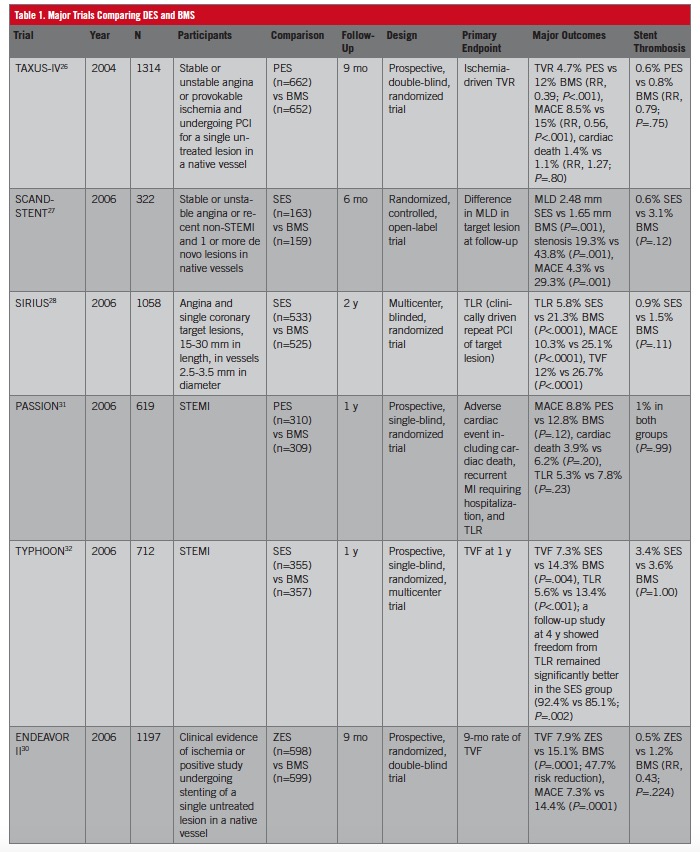
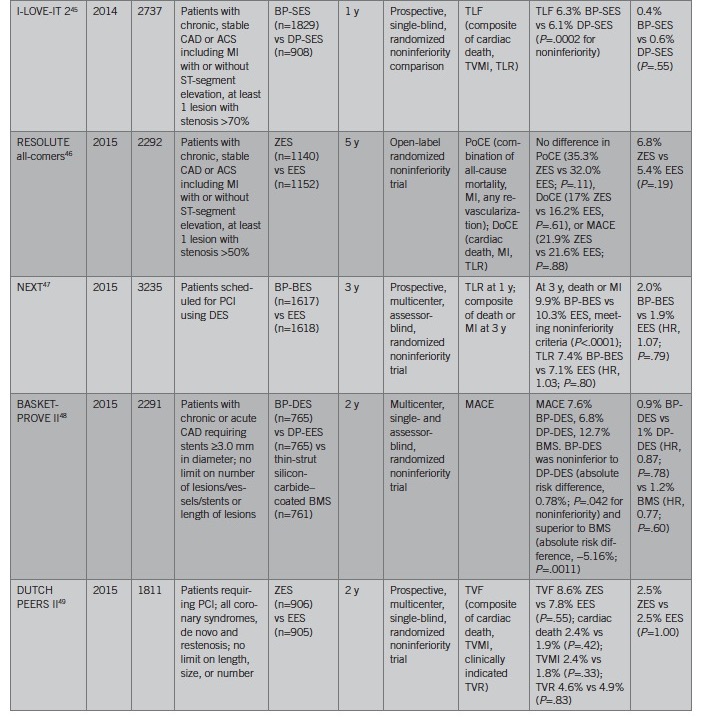
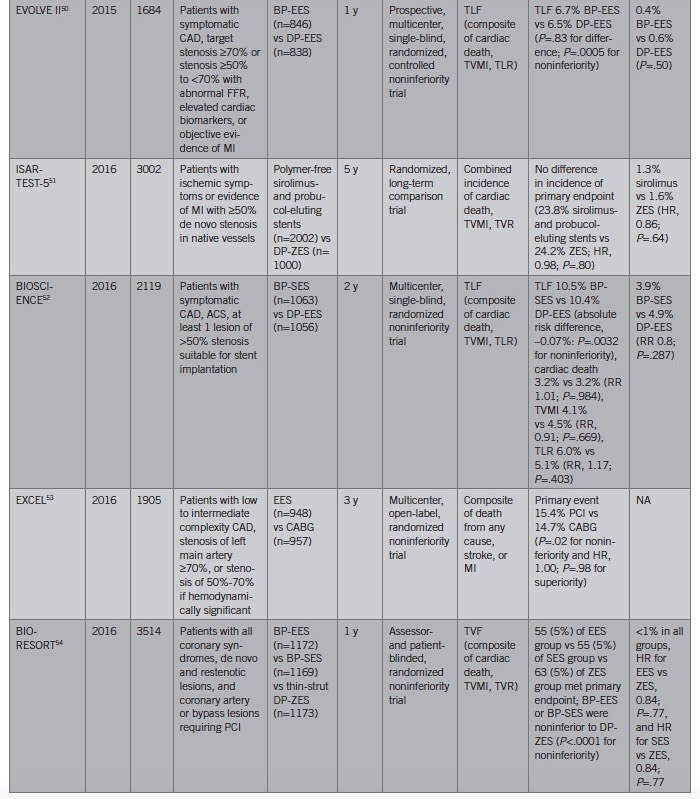
Even though stents eliminated the post-balloon–angioplasty recoil, the presence of the device itself, unfortunately, promotes restenosis by causing proliferation of vascular smooth-muscle cells. To reduce this neointimal hyperplasia, antiproliferative drugs were coated onto the metal scaffolds, and thus began the generation of drug-eluting stents (DES). Major trials showed the superiority of DES over bare-metal stents (BMS) (Table 1), with the need for repeated revascularization reduced by 50% to 70%.26-30 A DES includes a polymer layer (long-chain macromolecules) in addition to the metallic strut (as in a BMS). The polymer acts as the vehicle for and ensures a controlled release of the antiproliferative drugs, depending upon the drug-polymer binding and partition coefficient of the drug in the polymer.
DRUGS USED IN DRUG-ELUTING STENTS
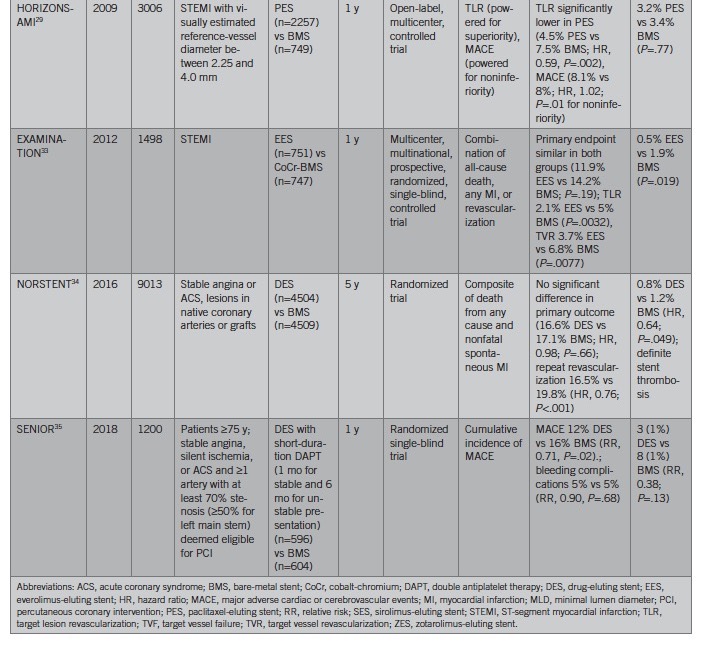
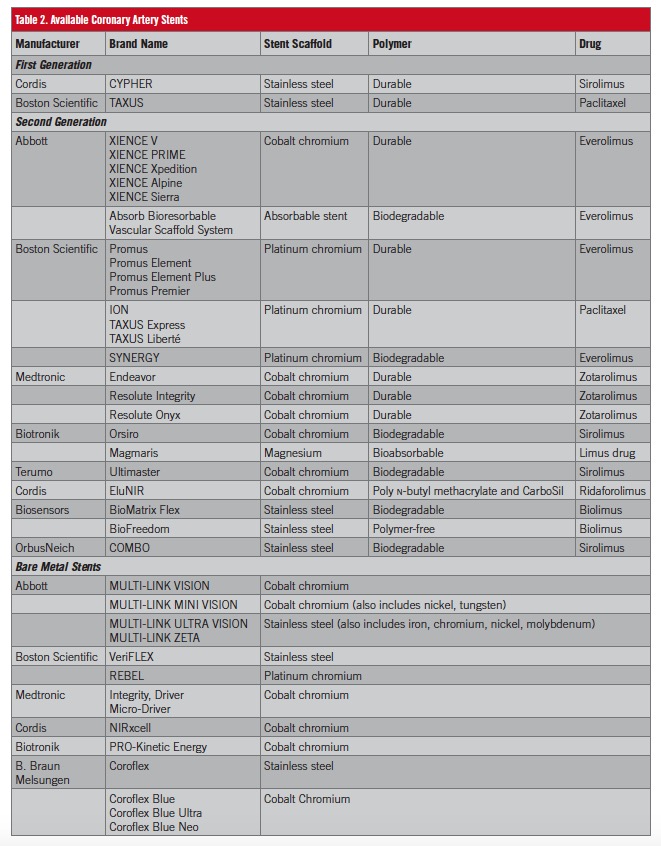
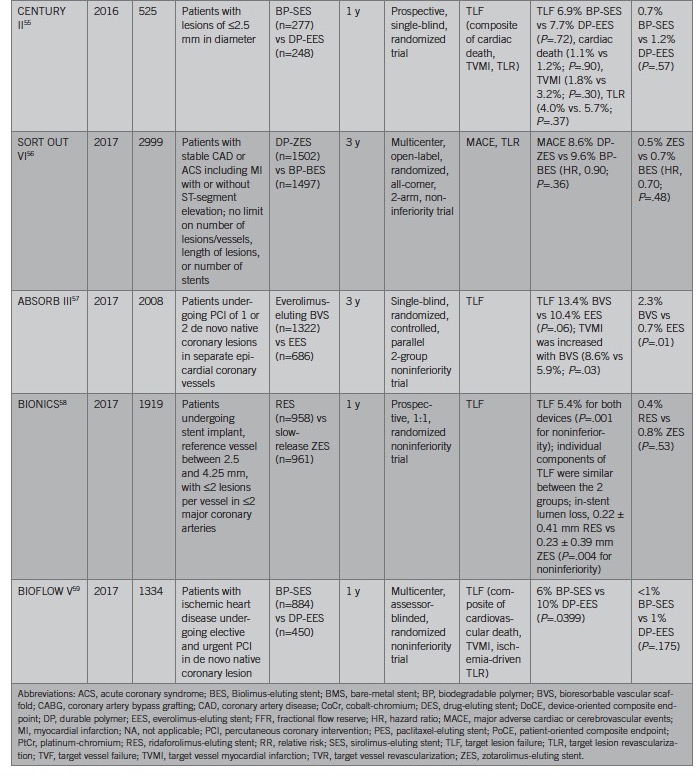
The two most clinically important classes of antiproliferative agents are paclitaxel and sirolimus analogues. Paclitaxel primarily stabilizes intracellular microtubules and arrests mitosis and thus cell proliferation.36,37 Sirolimus was initially isolated as an antifungal agent from a strain of Streptomyces hygroscopicus. Subsequent studies revealed its impressive antiproliferative properties—it blocks the activation of the cell-cycle–specific kinase, ultimately blocking the cell-cycle progression in the mid to late G1 phase.37 Multiple analogues of sirolimus have been developed, including zotarolimus, everolimus, umirolimus (Biolimus), novolimus, myolimus, and Amphilimus (sirolimus plus fatty acid). Accordingly, several different DES are available (Table 2), and numerous clinical trials have evaluated their efficacy (Table 3).
First-Generation Drug-Eluting Stents
The first-generation DES include the Cypher (sirolimus-eluting stent) and the Taxus (paclitaxel-eluting stent), which were the first two devices approved for clinical use in the United States by the Food and Drug Administration (FDA). Both devices were based on existing BMS platforms coupled with nonbiodegradable polymers.
Second-Generation Drug-Eluting Stents
Second-generation DES are more refined. They have thinner struts composed of cobalt-chromium or platinum-chromium alloys. Among the common second-generation DES are Endeavor, Resolute, Xience, and Promus series.60 The Endeavor stent consists of a phosphorylcholine/zotarolimus coating applied to the cobalt-chromium metallic scaffold. Drug elution is relatively rapid, with 100% of zotarolimus released within 30 days. It received FDA approval in 2008 based on the findings of ENDEAVOR series of clinical trials.40,41 Likewise, the Resolute DES also contains zotarolimus, but instead of the phosphorylcholine polymer, it has a tripolymer consisting of both hydrophobic and hydrophilic components, and approximately 60% of drug is released within 30 days.60
The Xience stent series contains everolimus and consists of a durable fluorinated copolymer matrix on a cobalt-chromium stent. Approximately 80% of the drug is released after 30 days. The SPIRIT series of trials evaluated the safety and efficacy of the Xience system.39,44 It was also FDA-approved in 2008. The Promus family of everolimus-eluting stents also has the identical fluorinated polymer as the Xience devices. However, the stent platform is based on the Omega platinum-chromium stent. The PLATINUM trial established Promus as noninferior to Xience V in regard to the primary endpoint of target vessel failure.43
Biodegradable Polymers
While polymers are crucial in effective drug delivery, their persistence may also elicit inflammatory responses, leading to late and very late stent thrombosis, as well as stenosis.60 Thus, there has been great interest in DES with biodegradable polymers and even novel polymer-free DES. The Synergy everolimus-eluting stent is based on the platinum-chromium platform. However, the polymer coating is composed of biodegradable poly(d,l-lactide-coglycolide) (PDLGA). The PDLGA polymer is fully absorbed after 3 to 4 months, eliminating long-term polymer exposure. It was approved in the United States in 2015 based on the pivotal EVOLVE II study, which showed the Synergy stent to be noninferior to the Promus Element Plus in regard to target lesion failure at 12 months.50
Bioresorbable Drug-Eluting Stents
Despite improved efficacy with DES, late stent thrombosis and target lesion revascularization still remain major concerns.61,62 The continued presence of metallic struts can promote in-stent neoatherosclerosis, recurrent stent thrombosis, and restenosis.63 Thus, the idea of bioresorbable scaffolds has gained much interest, given that they could offer potential advantages in restoring natural vascular structure and function.64-68 The resorption of the stent could make future revascularization easier if needed, especially in cases with side branches. Absorb everolimus-eluting poly-l-lactic acid–based bioresorbable vascular scaffold (BVS) was the first completely bioresorbable DES brought into clinical use. It was FDA-approved in 2016 but was later commercially withdrawn when follow-up data showed more harm with BVS. The ABSORB II trial randomly assigned 501 patients in a 2 to 1 ratio to receive either the Absorb BVS or Xience DES.65 At 3 years of follow-up, the Absorb BVS did not meet the primary outcome of the restoration of vasomotor activity (superiority trial) or late luminal loss (inferiority criteria). Likewise, the ABSORB III trial, which had a larger sample size, evaluated 3-year clinical outcomes of the Absorb BVS and reported higher rates of target vessel MI (8.6% vs 5.9%, P=.03) and device thrombosis (2.3% vs 0.7%, P=.01) compared with cobalt-chromium everolimus-eluting stents.57,69
CONCLUSION
The history and evolution of coronary artery stenting are among the most remarkable aspects of modern medicine. Today, coronary artery stents are the treatment of choice for CAD, supported by a large number of efficacy and safety studies. However, stent restenosis and thrombosis still remain a significant challenge for modern coronary artery stents.
REFERENCES:
- Gilbert RE. Eisenhower’s 1955 heart attack: medical treatment, political effects, and “behind the scenes” leadership style. Politics Life Sci. 2008;27(1):2-21. doi:10.2990/27_1_2
- Messerli FH, Messerli AW, Lüscher TF. Eisenhower’s billion-dollar heart attack—50 years later. N Engl J Med. 2005;353(12):1205-1207. doi:10.1056/NEJMp058162
- Monagan D. Journey Into the Heart. A Tale of Pioneering Doctors and Their Race to Transform Cardiovascular Medicine. New York, NY: Penguin Group (USA) Inc; 2007.
- Forssmann-Falch R. Werner Forssmann: a pioneer of cardiology. Am J Cardiol. 1997;79(5):651-660. doi:10.1016/s0002-9149(96)00833-8
- King SB III. The development of interventional cardiology. J Am Coll Cardiol. 1998;31(4 suppl 2):64B-88B. doi:10.1016/s0735-1097(97)00558-5
- The Nobel Prize in Physiology or Medicine 1956. Nobel Prize website. https://www.nobelprize.org/prizes/medicine/1956/summary/. Accessed February 26, 2020.
- Cowley MJ. Tribute to a legend in invasive/interventional cardiology Melvin P. Judkins, M.D. (1922–85). Catheter Cardiovasc Interv. 2005;64(2):259-261. doi:10.1002/ccd.20279
- Kinney TB. Radiologic history exhibit. Charles T. Dotter: a pioneering interventional radiologist. Radiographics. 1996;16(3):697-707. doi:10.1148/radiographics.16.3.8897633
- Doby T. A tribute to Sven-Ivar Seldinger. AJR Am J Roentgenol. 1984;142(1):1-4. doi:10.2214/ajr.142.1.1
- Payne MM. Charles Theodore Dotter: the father of intervention. Tex Heart Inst J. 2001;28(1):28-38.
- Forrester JS. The Heart Healers: The Misfits, Mavericks, and Rebels Who Created the Greatest Medical Breakthrough of Our Lives. New York, NY: St. Martin’s Press; 2015.
- Barton M, Grüntzig J, Husmann M, Rösch J. Balloon angioplasty—the Legacy of Andreas Grüntzig, M.D. (1939–1985). Front Cardiovasc Med. 2014;1:15. doi:10.3389/fcvm.2014.00015
- Kahn JK. Geoffrey O. Hartzler. Clin Cardiol. 2004;27(1):58-59. doi:10.1002/clc.4960270115
- Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996;335(4):217-225. doi:10.1056/NEJM199607253350401
- RITA Trial Participants. Coronary angioplasty versus coronary artery bypass surgery: the Randomized Intervention Treatment of Angina (RITA) trial. Lancet. 1993;341(8845):573-580.
- CABRI Trial Participants. First-year results of CABRI (Coronary Angioplasty versus Bypass Revascularisation Investigation). Lancet. 1995;346(8984):1179-1184.
- Hamm CW, Reimers J, Ischinger T, Rupprecht H-J, Berger J, Bleifeld W; German Angioplasty Bypass Surgery Investigation. A randomized study of coronary angioplasty compared with bypass surgery in patients with symptomatic multivessel coronary disease. N Engl J Med. 1994;331(16):1037-1043. doi:10.1056/NEJM199410203311601
- King SB III, Lembo NJ, Weintraub WS, et al; Emory Angioplasty versus Surgery Trial (EAST). A randomized trial comparing coronary angioplasty with coronary bypass surgery. N Engl J Med. 1994;331(16):1044-1050. doi:10.1056/NEJM199410203311602
- Mauri L, Bonan R, Weiner BH, et al. Cutting balloon angioplasty for the prevention of restenosis: results of the Cutting Balloon Global Randomized Trial. Am J Cardiol. 2002;90(10):1079-1083. doi:10.1016/s0002-9149(02)02773-x
- Albiero R, Silber S, Di Mario C, et al; RESCUT Investigators. Cutting balloon versus conventional balloon angioplasty for the treatment of in-stent restenosis: results of the Restenosis Cutting Balloon Evaluation Trial (RESCUT). J Am Coll Cardiol. 2004;43(6):943-949. doi:10.1016/j.jacc.2003.09.054
- Serruys PW, Luijten HE, Beatt KJ, et al. Incidence of restenosis after successful coronary angioplasty: a time-related phenomenon. A quantitative angiographic study in 342 consecutive patients at 1, 2, 3, and 4 months. Circulation. 1988;77(2):361-371. doi:10.1161/01.cir.77.2.361
- Sigwart U, Puel J, Mirkovitch V, Joffre F, Kappenberger L. Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty. N Engl J Med. 1987;316(12):701-706. doi:10.1056/NEJM198703193161201
- Fischman DL, Leon MB, Baim DS, et al; Stent Restenosis Study Investigators. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. N Engl J Med. 1994;331(8):496-501. doi:10.1056/NEJM199408253310802
- Serruys PW, de Jaegere P, Kiemeneij F, et al; Benestent Study Group. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. N Engl J Med. 1994;331(8):489-495. doi:10.1056/NEJM199408253310801
- Kastrati A, Mehilli J, Dirschinger J, et al. Intracoronary stenting and angiographic results: Strut Thickness Effect on Restenosis Outcome (ISAR-STEREO) trial. Circulation. 2001;103(23):2816-2821. doi:10.1161/01.cir.103.23.2816
- Stone GW, Ellis SG, Cox DA, et al; TAXUS-IV Investigators. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting TAXUS stent: the TAXUS-IV trial. Circulation. 2004;109(16):1942-1947. doi:10.1161/01.CIR.0000127110.49192.72
- Kelbæk H, Thuesen L, Helqvist S, et al; SCANDSTENT Investigators. The Stenting Coronary Arteries in Non-stress/benestent Disease (SCANDSTENT) Trial. J Am Coll Cardiol. 2006;47(2):449-455. doi:10.1016/j.jacc.2005.10.045
- Weisz G, Leon MB, Holmes DR Jr, et al. Two-year outcomes after sirolimus-eluting stent implantation: results from the Sirolimus-Eluting Stent in de Novo Native Coronary Lesions (SIRIUS) Trial. J Am Coll Cardiol. 2006;47(7):1350-1355. doi:10.1016/j.jacc.2005.11.077
- Stone GW, Lansky AJ, Pocock SJ, et al; HORIZONS-AMI Trial Investigators. Paclitaxel-eluting stents versus bare-metal stents in acute myocardial infarction. N Engl J Med. 2009;360(19):1946-1959. doi:10.1056/NEJMoa0810116
- Fajadet J, Wijns W, Laarman GJ, et al; ENDEAVOR II Investigators. Randomized, double-blind multicenter study of the Endeavor zotarolimus-eluting phosphorylcholine-encapsulated stent for treatment of native coronary artery lesions: clinical and angiographic results of the ENDEAVOR II trial. Circulation. 2006;114(8):798-806. doi:10.1161/CIRCULATIONAHA.105.591206
- Laarman GJ, Suttorp MJ, Dirksen MT, et al. Paclitaxel-eluting versus uncoated stents in primary percutaneous coronary intervention. N Engl J Med. 2006;355(11):1105-1113. doi:10.1056/NEJMoa062598
- Spaulding C, Henry P, Teiger E, et al; TYPHOON Investigators. Sirolimus-eluting versus uncoated stents in acute myocardial infarction. N Engl J Med. 2006;355(11):1093-1104. doi:10.1056/NEJMoa062006
- Sabate M, Cequier A, Iñiguez A, et al. Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (EXAMINATION): 1 year results of a randomised controlled trial. Lancet. 2012;380(9852):1482-1490. doi:10.1016/S0140-6736(12)61223-9
- Bønaa KH, Mannsverk J, Wiseth R, et al; NORSTENT Investigators. Drug-eluting or bare-metal stents for coronary artery disease. N Engl J Med. 2016;375(13):1242-1252. doi:10.1056/NEJMoa1607991
- Varenne O, Cook S, Sideris G, et al; SENIOR Investigators. Drug-eluting stents in elderly patients with coronary artery disease (SENIOR): a randomised single-blind trial. Lancet. 2018;391(10115):41-50. doi:10.1016/S0140-6736(17)32713-7
- Byrne RA, Stone GW, Ormiston J, Kastrati A. Coronary balloon angioplasty, stents, and scaffolds. Lancet. 2017;390(10096):781-792. doi:10.1016/S0140-6736(17)31927-X
- Sehgal SN. Rapamune® (RAPA, rapamycin, sirolimus): mechanism of action immunosuppressive effect results from blockade of signal transduction and inhibition of cell cycle progression. Clin Biochem. 1998;31(5):335-340. doi:10.1016/s0009-9120(98)00045-9
- Serruys PW, Morice M-C, Kappetein AP, et al; SYNTAX Investigators. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961-972. doi:10.1056/NEJMoa0804626
- Stone GW, Midei M, Newman W, et al; SPIRIT III Investigators. Randomized comparison of everolimus-eluting and paclitaxel-eluting stents: two-year clinical follow-up from the Clinical Evaluation of the Xience V Everolimus Eluting Coronary Stent System in the Treatment of Patients with de novo Native Coronary Artery Lesions (SPIRIT) III trial. Circulation. 2009;119(5):680-686. doi:10.1161/CIRCULATIONAHA.108.803528
- Leon MB, Mauri L, Popma JJ, et al. A randomized comparison of the Endeavor zotarolimus-eluting stent versus the TAXUS paclitaxel-eluting stent in de novo native coronary lesions: 12-month outcomes from the ENDEAVOR IV trial. J Am Coll Cardiol. 2010;55(6):543-554. doi:10.1016/j.jacc.2009.08.067
- Kirtane AJ, Leon MB, Ball MW, et al; ENDEAVOR IV Investigators. The “final” 5-year follow-up from the ENDEAVOR IV trial comparing a zotarolimus-eluting stent with a paclitaxel-eluting stent. JACC Cardiovasc Interv. 2013;6(4):325-333. doi:10.1016/j.jcin.2012.12.123
- Smits PC, Kedhi E, Royaards K-J, et al. 2-year follow-up of a randomized controlled trial of everolimus- and paclitaxel-eluting stents for coronary revascularization in daily practice. COMPARE (Comparison of the everolimus eluting XIENCE-V stent with the paclitaxel eluting TAXUS LIBERTÉ stent in all-comers: a randomized open label trial). J Am Coll Cardiol. 2011;58(1):11-18. doi:10.1016/j.jacc.2011.02.023
- Stone GW, Teirstein PS, Meredith IT, et al; PLATINUM Trial Investigators. A prospective randomized evaluation of a novel everolimus-eluting coronary stent: the PLATINUM (A Prospective, Randomized, Multicenter Trial to Assess an Everolimus-Eluting Coronary Stent System [PROMUS Element] for the Treatment of up to Two De Novo Coronary Artery Lesions) trial. J Am Coll Cardiol. 2011;57(16):1700-1708. doi:10.1016/j.jacc.2011.02.016
- Stone GW, Rizvi A, Sudhir K, et al; SPIRIT IV Investigators. Randomized comparison of everolimus- and paclitaxel-eluting stents: 2-year follow-up from the SPIRIT (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System) IV trial. J Am Coll Cardiol. 2011;58(1):19-25. doi:10.1016/j.jacc.2011.02.022
- Han Y, Xu B, Jing Q, et al; I-LOVE-IT 2 Investigators. A randomized comparison of novel biodegradable polymer- and durable polymer–coated cobalt-chromium sirolimus-eluting stents. JACC Cardiovasc Interv. 2014;7(12):1352-1360. doi:10.1016/j.jcin.2014.09.001
- Iqbal J, Serruys PW, Silber S, et al. Comparison of zotarolimus- and everolimus-eluting coronary stents: final 5-year report of the RESOLUTE all-comers trial. Circ Cardiovasc Interv. 2015;8(6):e002230. doi:10.1161/CIRCINTERVENTIONS.114.002230
- Natsuaki M, Kozuma K, Morimoto T, et al. Final 3-year outcome of a randomized trial comparing second-generation drug-eluting stents using either biodegradable polymer or durable polymer: NOBORI biolimus-eluting versus XIENCE/PROMUS everolimus-eluting stent trial. Circ Cardiovasc Interv. 2015;8(10):e002817. doi:10.1161/CIRCINTERVENTIONS.115.002817
- Kaiser C, Galatius S, Jeger R, et al; BASKET-PROVE II Study Group. Long-term efficacy and safety of biodegradable-polymer biolimus-eluting stents: main results of the Basel Stent Kosten-Effektivitäts Trial—PROspective Validation Examination II (BASKET-PROVE II), a randomized, controlled noninferiority 2-year outcome trial. Circulation. 2015;131(1):74-81. doi:10.1161/CIRCULATIONAHA.114.013520
- Sen H, Lam MK, Löwik MM, et al. Clinical events and patient-reported chest pain in all-comers treated with resolute integrity and Promus Element stents: 2-year follow-up of the DUTCH PEERS (DUrable polymer-based STent CHallenge of Promus ElemEnt versus ReSolute Integrity) randomized trial (TWENTE II). JACC Cardiovasc Interv. 2015;8(7):889-899. doi:10.1016/j.jcin.2015.01.033
- Kereiakes DJ, Meredith IT, Windecker S, et al. Efficacy and safety of a novel bioabsorbable polymer-coated, everolimus-eluting coronary stent: the EVOLVE II Randomized Trial. Circ Cardiovasc Interv. 2015;8(4):e002372. doi:10.1161/CIRCINTERVENTIONS.114.002372
- Kufner S, Sorges J, Mehilli J, et al; ISAR-TEST-5 Investigators. Randomized trial of polymer-free sirolimus- and probucol-eluting stents versus durable polymer zotarolimus-eluting stents: 5-year results of the ISAR-TEST-5 trial. JACC Cardiovasc Interv. 2016;9(8):784-792. doi:10.1016/j.jcin.2016.01.009
- Zbinden R, Piccolo R, Heg D, et al. Ultrathin strut biodegradable polymer sirolimus-eluting stent versus durable-polymer everolimus-eluting stent for percutaneous coronary revascularization: 2-year results of the BIOSCIENCE trial. J Am Heart Assoc. 2016;5(3):e003255. doi:10.1161/JAHA.116.003255
- Stone GW, Sabik JF, Serruys PW, et al; EXCEL Trial Investigators. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med. 2016;375(23):2223-2235. doi:10.1056/NEJMoa1610227
- von Birgelen C, Kok MM, van der Heijden LC, et al. Very thin strut biodegradable polymer everolimus-eluting and sirolimus-eluting stents versus durable polymer zotarolimus-eluting stents in allcomers with coronary artery disease (BIO-RESORT): a three-arm, randomised, non-inferiority trial. Lancet. 2016;388(10060):2607-2617. doi:10.1016/S0140-6736(16)31920-1
- Wöhrle J, Markovic S, Rottbauer W, et al; CENTURY II Investigators. Bioresorbable polymer sirolimus-eluting coronary stent compared with permanent polymer everolimus-eluting coronary stent implantation for treatment of small vessel coronary artery disease: CENTURY II trial. EuroIntervention. 2016;12(2):e167-e174. doi:10.4244/EIJV12I2A30
- Raungaard B, Christiansen EH, Bøtker HE, et al; SORT OUT VI Investigators. Comparison of durable-polymer zotarolimus-eluting and biodegradable-polymer biolimus-eluting coronary stents in patients with coronary artery disease: 3-year clinical outcomes in the randomized SORT OUT VI trial. JACC Cardiovasc Interv. 2017;10(3):255-264. doi:10.1016/j.jcin.2016.11.007
- Kereiakes DJ, Ellis SG, Metzger C, et al; ABSORB III Investigators. 3-Year clinical outcomes with everolimus-eluting bioresorbable coronary scaffolds: the ABSORB III trial. J Am Coll Cardiol. 2017;70(23):2852-2862. doi:10.1016/j.jacc.2017.10.010
- Kandzari DE, Smits PC, Love MP, et al. Randomized comparison of ridaforolimus- and zotarolimus-eluting coronary stents in patients with coronary artery disease: primary results from the BIONICS trial (BioNIR Ridaforolimus-Eluting Coronary Stent System in Coronary Stenosis). Circulation. 2017;136(14):1304-1314. doi:10.1161/CIRCULATIONAHA.117.028885
- Kandzari DE, Mauri L, Koolen JJ, et al; BIOFLOW V Investigators. Ultrathin, bioresorbable polymer sirolimus-eluting stents versus thin, durable polymer everolimus-eluting stents in patients undergoing coronary revascularisation (BIOFLOW V): a randomised trial. Lancet. 2017;390(10105):1843-1852. doi:10.1016/S0140-6736(17)32249-3
- Chen C-H, Kirtane AJ. Stents, restenosis, and stent thrombosis. In: Kern MJ, Lim MJ, Sorajja P, eds. The Interventional Cardiac Catheterization Handbook. 4th ed. Elsevier; 2018:chap 6.
- Natsuaki M, Morimoto T, Furukawa Y, et al; CREDO-Kyoto PCI/CABG Registry Cohort-2 Investigators. Late adverse events after implantation of sirolimus-eluting stent and bare-metal stent: long-term (5-7 years) follow-up of the Coronary Revascularization Demonstrating Outcome study-Kyoto registry Cohort-2. Circ Cardiovasc Interv. 2014;7(2):168-179. doi:10.1161/CIRCINTERVENTIONS.113.000987
- Camenzind E, Wijns W, Mauri L, et al; PROTECT Steering Committee and Investigators. Stent thrombosis and major clinical events at 3 years after zotarolimus-eluting or sirolimus-eluting coronary stent implantation: a randomised, multicentre, open-label, controlled trial. Lancet. 2012;380(9851):1396-1405. doi:10.1016/S0140-6736(12)61336-1
- Otsuka F, Byrne RA, Yahagi K, et al. Neoatherosclerosis: overview of histopathologic findings and implications for intravascular imaging assessment. Eur Heart J. 2015;36(32):2147-2159. doi:10.1093/eurheartj/ehv205
- Wykrzykowska JJ, Kraak RP, Hofma SH, et al; AIDA Investigators. Bioresorbable scaffolds versus metallic stents in routine PCI. N Engl J Med. 2017;376(24):2319-2328. doi:10.1056/NEJMoa1614954
- Serruys PW, Chevalier B, Sotomi Y, et al. Comparison of an everolimus-eluting bioresorbable scaffold with an everolimus-eluting metallic stent for the treatment of coronary artery stenosis (ABSORB II): a 3 year, randomised, controlled, single-blind, multicentre clinical trial. Lancet. 2016;388(10059):2479-2491. doi:10.1016/S0140-6736(16)32050-5
- Haude M, Ince H, Abizaid A, et al. Safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de-novo coronary artery lesions (BIOSOLVE-II): 6 month results of a prospective, multicentre, non-randomised, first-in-man trial. Lancet. 2016;387(10013):31-39. doi:10.1016/S0140-6736(15)00447-X
- Serruys PW, Ormiston J, van Geuns R-J, et al. A polylactide bioresorbable scaffold eluting everolimus for treatment of coronary stenosis: 5-year follow-up. J Am Coll Cardiol. 2016;67(7):766-776. doi:10.1016/j.jacc.2015.11.060
- Cassese S, Byrne RA, Ndrepepa G, et al. Everolimus-eluting bioresorbable vascular scaffolds versus everolimus-eluting metallic stents: a meta-analysis of randomised controlled trials. Lancet. 2016;387(10018):537-544. doi:10.1016/S0140-6736(15)00979-4
- Ellis SG. Everolimus-eluting bioresorbable vascular scaffolds in patients with coronary artery disease: ABSORB III trial 2-year results. Presented at: American College of Cardiology 2017 Scientific Session; March 19, 2017; Washington, DC. https://www.tctmd.com/slide/everolimus-eluting-bioresorbable-vascular-scaffolds-patients-coronary-artery-disease-absorb. Accessed February 26, 2020.


